The AI Revolution: Reshaping Healthcare in 2025
Artificial intelligence is no longer just a futuristic concept in medicine; it's a present-day force actively transforming patient outcomes. Understanding the diverse AI applications in healthcare is becoming essential for anyone curious about technology's impact or looking to innovate. This listicle cuts to the chase, presenting 10 pivotal ways AI is already revolutionizing areas from diagnostics and drug discovery to personalized treatments and public health by 2025. Discover how these intelligent systems are making healthcare smarter, faster, and more accessible, offering a clear roadmap to the future of medical practice.
1. Medical Imaging and Diagnostics
One of the most impactful and rapidly advancing AI applications in healthcare is in the realm of Medical Imaging and Diagnostics. Imagine having a highly skilled assistant who can analyze medical scans with incredible speed and precision, often spotting subtle clues that might elude the human eye. That's essentially what AI brings to radiology departments around the world. This technology leverages sophisticated deep learning algorithms, a subset of machine learning, to scrutinize radiological images. These aren't just any images; we're talking about X-rays, CT scans, MRIs, and mammograms – the cornerstones of modern diagnostic medicine.
How does it work? At its core, AI-powered medical imaging trains computer vision models on vast datasets of annotated medical images. These datasets contain thousands, sometimes millions, of scans where experts have already identified specific conditions or abnormalities. The algorithms learn to recognize complex patterns, textures, and anomalies associated with various diseases, much like a human radiologist does, but with the potential for greater consistency and speed. For instance, an AI might learn to identify the tell-tale signs of early-stage lung cancer on a chest X-ray or detect minute microcalcifications on a mammogram that could indicate breast cancer. This capability is particularly crucial for early-stage disease detection, where prompt diagnosis can dramatically improve patient outcomes.
This field truly deserves its prominent place in discussions about AI applications in healthcare because it directly addresses critical challenges: improving diagnostic accuracy, accelerating the diagnostic process, and making expert-level analysis more accessible.
Key features that make AI invaluable in this domain include:
- Automated detection of abnormalities: AI systems can flag suspicious areas in medical images for further review by radiologists.
- Pattern recognition capabilities: In specific, well-defined tasks, these models can achieve, and sometimes exceed, human accuracy in identifying diseases.
- Integration with existing PACS: Modern AI tools are often designed to seamlessly integrate with Picture Archiving and Communication Systems (PACS), which hospitals already use to store and manage medical images. This ensures a smooth workflow for healthcare professionals.
- Real-time analysis and instant results: While not always fully autonomous, AI can provide preliminary findings in minutes, which is critical in emergency situations.
- Multi-modal imaging analysis: Some advanced AI systems can synthesize information from different types of scans (e.g., combining MRI and CT data) to provide a more comprehensive diagnostic picture.
The benefits are compelling. We're seeing improved diagnostic accuracy, especially for conditions like early-stage cancers where subtle signs are paramount. Interpretation times can be drastically reduced from hours to minutes, freeing up radiologists to focus on more complex cases and patient interaction. The 24/7 availability of AI tools can be a lifesaver for emergency diagnostics when human specialists might be less readily available. Furthermore, AI introduces standardized analysis, which helps in reducing human error and inherent biases, leading to more consistent diagnostic quality. Over time, this efficiency can also contribute to cost reduction in healthcare delivery.
However, the adoption of AI in medical imaging is not without its challenges. The high initial implementation costs for software, hardware, and integration can be a barrier for some healthcare facilities. These systems require extensive training data and rigorous validation to ensure they are safe and effective across diverse patient populations. The regulatory approval processes for medical AI devices (like FDA clearance in the US) can be lengthy and complex, slowing down the deployment of new technologies. There's also a valid concern about the risk of over-reliance on technology, potentially deskilling radiologists or leading to complacency. Finally, AI's effectiveness can be limited for rare conditions where insufficient training data exists, making it hard for the algorithms to learn reliable patterns.
To better understand the significant impact of AI in medical imaging, the following bar chart visualizes key comparative metrics and market projections.
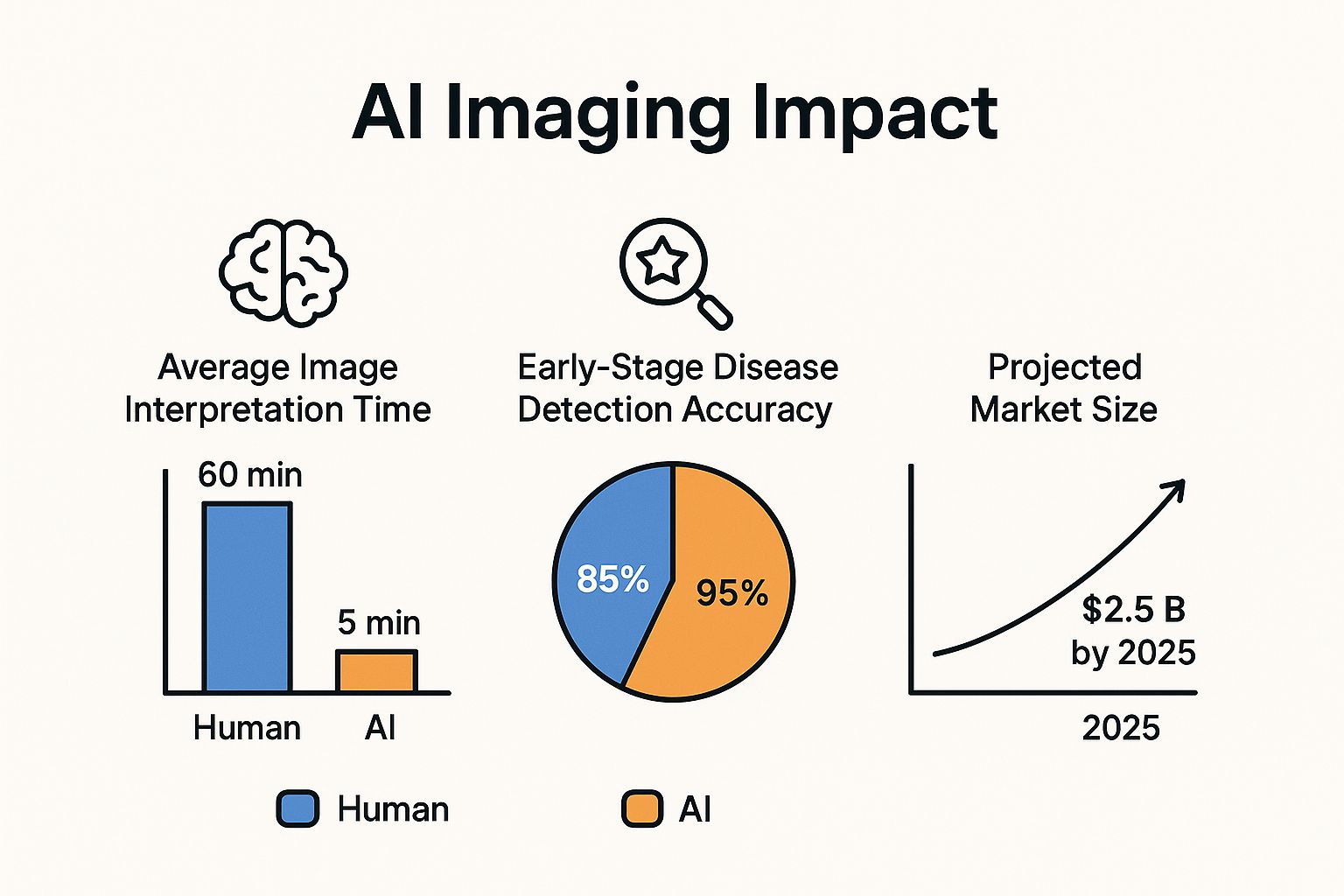 This chart clearly illustrates the transformative potential of AI, showcasing a dramatic reduction in average image interpretation time from 60 minutes for humans to just 5 minutes for AI, a significant boost in early-stage disease detection accuracy from 85% to 95%, and a projected market size for AI imaging reaching $2.5 billion by 2025.
This chart clearly illustrates the transformative potential of AI, showcasing a dramatic reduction in average image interpretation time from 60 minutes for humans to just 5 minutes for AI, a significant boost in early-stage disease detection accuracy from 85% to 95%, and a projected market size for AI imaging reaching $2.5 billion by 2025.
Numerous success stories highlight the real-world impact of these AI applications in healthcare. For instance, Google's DeepMind has demonstrated AI that can detect over 50 eye diseases from Optical Coherence Tomography (OCT) scans with an accuracy comparable to leading experts. Companies like Zebra Medical Vision (now part of Nanox AI) developed the "AI1" bundle, offering automated analysis for various findings in radiology. Aidoc has gained recognition for its AI solutions that prioritize critical cases like stroke detection in head CT scans, alerting physicians almost instantaneously. IBM Watson for Oncology has also been explored for its capabilities in analyzing medical images for cancer diagnosis, and PathAI is making strides in using machine learning for pathology diagnosis from digital slide images.
So, when and why should healthcare providers consider this approach? AI in medical imaging is particularly beneficial for high-volume screening programs (like mammography or lung cancer screening), where it can act as a "second reader" or help triage cases. It's invaluable for initiatives focused on early disease detection, as AI can pick up on nascent signs. In busy departments, it can support radiologists by flagging urgent cases, reducing burnout, and improving workflow efficiency. For emergency diagnostics, especially in underserved areas or during off-hours, AI can provide crucial preliminary reads.
If you're considering integrating AI into your imaging workflows, here are some actionable tips:
- Start with pilot programs: Begin with specific imaging modalities or clinical questions to evaluate performance and workflow integration before a full-scale rollout.
- Ensure robust data governance and patient privacy protocols: Protecting sensitive patient data is paramount. Comply with regulations like HIPAA or GDPR.
- Invest in radiologist training for AI tool integration: Radiologists need to understand how the AI tools work, their strengths, and their limitations to use them effectively as part of their diagnostic process.
- Implement quality assurance processes for AI-generated results: Continuously monitor and validate the AI's performance to ensure accuracy and reliability.
- Choose FDA-approved or CE-marked solutions for clinical implementation: This ensures the tools have met stringent regulatory standards for safety and efficacy.
The popularization of AI in medical imaging owes much to pioneers like Geoffrey Hinton, whose work on deep learning laid the foundational algorithms. Researchers like Fei-Fei Li from Stanford AI Lab have significantly contributed to computer vision, which is central to image analysis. Teams at Google DeepMind, and innovative companies like Zebra Medical Vision (now Nanox AI) and the founders of Aidoc, have been instrumental in translating these technologies into practical, life-saving applications.
For a deeper dive into how AI is revolutionizing medical imaging, check out this insightful video:
In essence, AI is not looking to replace radiologists but rather to augment their capabilities, providing powerful tools to enhance diagnostic accuracy, speed, and efficiency, ultimately leading to better patient care and outcomes across numerous AI applications in healthcare.
2. Drug Discovery and Development
Bringing a new drug to market has traditionally been a marathon – a costly, lengthy journey often spanning 10-15 years and billions of dollars. Many promising candidates falter along the way. But AI is changing this, making drug discovery and development one of the most impactful AI applications in healthcare today by accelerating the process, reducing costs, and uncovering new treatments.
How AI Works to Revolutionize Drug Discovery
So, how exactly does AI supercharge this complex field? Essentially, AI, particularly machine learning (ML) models, analyzes immense biological and chemical datasets to identify patterns and predict outcomes much faster and more comprehensively than traditional methods. Think of it as an ultra-smart research assistant that can process and understand connections in data that might elude human researchers.
Key AI-driven capabilities transforming this domain include:
- Molecular Property Prediction and Optimization: AI algorithms can forecast how a molecule will behave in the human body—its effectiveness, potential toxicity, how it's absorbed or metabolized—often before it's even synthesized in a lab. This allows scientists to digitally tweak and optimize compound structures for better efficacy and safety profiles.
- Virtual Screening of Compound Libraries: Instead of painstakingly testing thousands, or even millions, of chemical compounds in physical labs (a process that can take years), AI can perform 'virtual screenings.' It rapidly analyzes vast digital libraries of molecules to identify those most likely to interact effectively with a specific disease target, drastically narrowing down the candidates for essential real-world testing.
- Target Identification and Validation: Finding the right 'target' in the body (like a specific protein or gene critically involved in a disease) is fundamental. AI helps identify novel biological targets by analyzing complex genomic, proteomic, and clinical data. It can also help validate whether interacting with this target will indeed produce a therapeutic effect.
- Clinical Trial Optimization and Patient Stratification: AI contributes to making clinical trials more efficient and successful. It assists in designing smarter trial protocols, predicting potential patient responses, and identifying the most suitable patient groups (patient stratification) who are likely to benefit from a particular drug. This not only improves success rates but can also reduce the time and cost of these crucial phases.
- Repurposing Existing Drugs for New Indications: Sometimes, a drug already approved and proven safe for one condition can be effective for an entirely different disease. AI excels at scanning existing drug databases, scientific literature, and real-world evidence to find these new therapeutic uses. This 'drug repurposing' offers a significantly faster and cheaper route to new treatments because the initial safety hurdles have already been cleared.
Why This Matters: The Monumental Impact
The integration of AI into drug discovery isn't just an incremental improvement; it's a paradigm shift. This is why it holds such a prominent place among AI applications in healthcare. The benefits are transformative:
- Drastically Reduced Timelines: AI has demonstrated the potential to slash the drug discovery timeline from the traditional 10-15 years down to an astonishing 3-5 years in some cases.
- Significantly Lower Development Costs: By identifying promising candidates earlier, predicting failures before costly experiments, and streamlining processes, AI can substantially cut down the immense financial burden of drug development.
- Higher Success Rates in Clinical Trials: Through improved target selection, better compound design, and more precise patient stratification, AI increases the likelihood that a drug candidate will prove safe and effective in clinical trials.
- Ability to Tackle Previously 'Undruggable' Targets: Some disease targets have been notoriously difficult to address with conventional drug discovery methods. AI's capacity to explore novel chemical spaces and understand complex biological interactions is opening doors to tackling these once 'undruggable' targets.
- Personalized Medicine Development: AI is instrumental in analyzing individual patient data (genomics, lifestyle, etc.) to help design or select drugs that are tailored to their specific biological makeup and disease characteristics, paving the way for truly personalized medicine.
Real-World Success Stories: AI in Action
This isn't just theoretical; AI is already delivering remarkable results, spearheaded by innovative companies and researchers:
- DeepMind's AlphaFold: Developed by Demis Hassabis's team at DeepMind (a Google AI company), AlphaFold revolutionized biology by accurately predicting the 3D structures of proteins from their amino acid sequences. Understanding a protein's structure is critical as it dictates its function, and this knowledge is foundational for designing drugs that can effectively interact with disease-related proteins.
- Atomwise's AI Platform: Atomwise, co-founded by Abraham Heifets, utilizes its AI platform (AtomNet®) for structure-based drug discovery. Notably, they rapidly identified potential drug candidates for COVID-19 by using AI to screen billions of compounds against viral protein targets.
- Insilico Medicine's AI-Designed Drug for Fibrosis: Led by Alex Zhavoronkov, Insilico Medicine made headlines by developing an AI-discovered and AI-designed drug for Idiopathic Pulmonary Fibrosis (IPF), which has progressed into Phase II clinical trials, showcasing a powerful end-to-end AI approach.
- BenevolentAI's Drug Repurposing for ALS: BenevolentAI, with pioneering figures like Jackie Hunter contributing to its vision, has successfully used its sophisticated AI platform to analyze biomedical information and identify existing drugs that could be repurposed for new diseases, including promising candidates for Amyotrophic Lateral Sclerosis (ALS).
- Recursion Pharmaceuticals' Automated Drug Discovery Platform: Co-founded by Chris Gibson, Recursion Pharmaceuticals employs a unique approach that combines AI with high-throughput, automated biology experiments. Their platform rapidly maps cellular responses to millions of drug candidates, accelerating the identification of potential treatments, especially for rare diseases and conditions like fibrosis.
The Flip Side: Challenges and Considerations
While the potential of AI in drug discovery is immense, it's important to acknowledge the hurdles:
- Limited by Quality and Completeness of Training Data: AI models are heavily dependent on the data they're trained on. High-quality, comprehensive, diverse, and unbiased datasets are crucial, and generating or accessing such data can be a significant challenge.
- Regulatory Uncertainty for AI-Discovered Drugs: The regulatory pathways for evaluating and approving drugs discovered or designed using AI are still evolving, creating some ambiguity for developers.
- High Computational Requirements: Training sophisticated AI models and performing large-scale virtual screenings can demand substantial computational power and resources.
- Need for Extensive Experimental Validation: AI predictions and identifications are powerful starting points, but they must always be validated through rigorous experimental testing in the lab and subsequently in human clinical trials.
- Intellectual Property Complexities: Determining ownership and patentability for discoveries where AI played a significant inventive role can present new legal and ethical questions.
Actionable Tips for Innovators and Enthusiasts
Inspired by these advancements? If you're an AI enthusiast, a hobbyist vibe builder, or someone exploring AI for go-to-market strategies or workflow automations (perhaps using tools like Replit, n8n, or Zapier in a biotech-adjacent context), here are some pointers:
- Prioritize Data Quality: If you're venturing into projects involving molecular or biological data, focus intensely on building or accessing comprehensive, high-quality, and well-curated databases. Data is the fuel for AI.
- Foster Collaboration: The intersection of AI and deep bioscience is complex. Seek collaborations with academic institutions, research organizations, or domain experts for biological expertise and crucial validation of findings.
- Embrace Hybrid Approaches: Don't aim to replace everything with AI overnight. Often, the most potent solutions emerge from combining AI's predictive power and pattern recognition capabilities with the nuanced insights from traditional experimental methods. To explore how you might integrate such powerful tools effectively, you can Learn more about Drug Discovery and Development.
- Navigate Regulatory Landscapes Early: If your work has the potential to lead to therapeutic applications, start thinking about regulatory compliance, ethical considerations, and safety standards from the very early stages of development.
- Focus Your Efforts: Drug discovery is an incredibly broad field. Consider focusing on specific therapeutic areas, particular types of diseases, or niche problems where AI can make a significant and demonstrable initial impact.
When and Why to Use This Approach
You'd typically leverage AI in drug discovery when facing challenges such as:
- High failure rates and attrition in traditional drug pipelines.
- An urgent need to accelerate development timelines, especially for emerging health crises or rare diseases with no existing treatments.
- Prohibitive costs associated with conventional R&D methods.
- Diseases with complex underlying biology where mechanisms are poorly understood or involve intricate molecular interactions.
- The imperative to discover novel classes of drugs or to find ways to target disease mechanisms previously considered "undruggable."
Essentially, AI is a powerful ally when you need to explore vast chemical and biological spaces, identify subtle but critical patterns in complex data, and make more informed decisions faster and more cost-effectively, ultimately aiming to bring life-saving medicines to patients sooner. This innovative use of AI applications in healthcare is not just promising; it's already delivering.
3. Personalized Treatment and Precision Medicine
Imagine a healthcare future where your treatment plan is as unique as your fingerprint. That's the promise of Personalized Treatment and Precision Medicine, a revolutionary approach supercharged by AI. Instead of one-size-fits-all solutions, this method leverages artificial intelligence to dive deep into a patient's specific data – think genetics, medical history, lifestyle choices, and even tiny biological clues called biomarkers – to recommend highly tailored treatment plans. The core idea is to match you with the most effective therapies based on your individual characteristics, significantly boosting the chances of a positive outcome. This is one of the most transformative ai applications in healthcare today.
How it Works & Key Features: So, how does AI make this personalized magic happen? It's all about data. AI algorithms sift through enormous, complex datasets—far beyond human capacity—to identify subtle patterns and correlations that predict how an individual might respond to therapy. This allows for a level of individualization previously unimaginable.
Key features that make this approach so powerful include:
- Genomic Data Analysis for Treatment Selection: AI deciphers your genetic code to pinpoint variations that might influence disease susceptibility or drug response. For example, in cancer care, AI can identify specific genetic mutations in a tumor, guiding oncologists to select targeted therapies that are most likely to be effective against those particular mutations.
- Biomarker Identification and Monitoring: Biomarkers are like signposts for your health – measurable indicators of a biological state or condition. AI excels at discovering novel biomarkers from complex data (like proteomics or metabolomics) and can continuously monitor existing ones to track disease progression or treatment effectiveness in real-time.
- Treatment Response Prediction: Before even starting a therapy, AI models can analyze your comprehensive data profile to predict how likely you are to respond positively, or if you might experience certain side effects. This predictive power is crucial for making informed treatment choices from the get-go.
- Adverse Reaction Risk Assessment: Similarly, AI can flag patients at higher risk of adverse drug reactions by analyzing their genetic predispositions and other health factors, allowing clinicians to choose safer alternatives or implement preventative measures.
- Dynamic Treatment Adjustment: Healthcare isn't static, and neither should treatment be. AI enables treatment plans to be fluid, adjusting them based on real-time data flowing in from wearables, monitoring devices, or follow-up tests, ensuring the treatment remains optimized as your condition evolves or new information becomes available.
Why This Approach is a Game-Changer: Personalized treatment and precision medicine, powered by AI, fundamentally shifts the paradigm from reactive to proactive and from generalized to individualized care. Its place in the landscape of ai applications in healthcare is cemented by its potential to make treatments more effective and safer. Instead of cycling through standard treatments hoping one will work, clinicians can use AI-driven insights to select the best initial therapy, saving precious time, reducing patient suffering, and improving overall outcomes. This targeted approach is particularly transformative for complex diseases like cancer, autoimmune disorders, or rare genetic conditions where individual variability plays a huge role in treatment success.
The Upsides: Pros of AI-Driven Precision Medicine The benefits are compelling and far-reaching, offering a significant leap forward in patient care:
- Improved treatment efficacy and reduced side effects: Tailoring treatments means hitting the disease target more accurately with less collateral damage to healthy cells, leading to better results with fewer unwanted effects.
- Better patient outcomes and quality of life: More effective treatments naturally lead to better health, faster recovery, and an improved ability to live life fully.
- Reduced healthcare costs: By minimizing trial-and-error, avoiding ineffective or harmful treatments, and potentially shortening treatment durations, targeted therapies can be more cost-effective in the long run.
- Accelerated development of rare disease treatments: AI can help identify patient subgroups within rare diseases who might benefit from specific investigational drugs, speeding up clinical trials and bringing hope to those with few options.
- Enhanced clinical decision-making support: AI acts as a sophisticated assistant to doctors, processing vast amounts of information to provide data-backed recommendations that augment their expertise and experience.
The Hurdles: Cons to Consider Despite its immense promise, the path to widespread AI-driven precision medicine has its challenges:
- Requires extensive patient data collection: The power of AI models depends on vast, high-quality, and diverse datasets, which can be difficult to gather, standardize, and manage.
- Privacy and security concerns with genetic information: Genetic data is inherently personal and highly sensitive, necessitating robust security measures, stringent access controls, and clear ethical guidelines to protect patient privacy.
- Health disparities may be amplified by biased datasets: If AI models are trained on data that doesn't adequately represent diverse populations (e.g., ethnic minorities, specific age groups), they may perpetuate or even worsen existing health inequities.
- High costs for genomic testing and analysis: The initial investment in genomic sequencing, sophisticated AI platforms, and the expertise to run them can be substantial, potentially limiting access.
- Complexity in integrating multiple data sources: Bringing together disparate data from EHRs, genomic labs, imaging systems, wearables, and lifestyle apps into a cohesive, analyzable format is a significant technical and logistical hurdle.
Real-World Success Stories: The impact of AI in precision medicine isn't just theoretical; it's already making a difference in clinics and research labs:
- IBM Watson for Oncology: While its journey has involved continuous learning and refinement, Watson for Oncology aims to provide oncologists with personalized, evidence-based cancer treatment options by analyzing a patient's medical information against a vast database of medical literature, treatment guidelines, and clinical trials.
- Foundation Medicine: This company offers comprehensive genomic profiling tests (like FoundationOne CDx) that analyze a patient's tumor DNA to identify specific genomic alterations. This information helps guide oncologists in selecting targeted therapies or immunotherapy for various cancers.
- Tempus Platform: Tempus is building a massive library of de-identified clinical and molecular data, coupled with an AI-driven operating system, to make data more accessible and useful for physicians to personalize cancer care and for researchers to accelerate discovery.
- 23andMe Pharmacogenomics Reports: While primarily known as a direct-to-consumer genetic testing company, 23andMe provides FDA-authorized reports on how an individual's genetics might influence their body's response to certain medications (pharmacogenomics), aiding in safer prescribing.
- Guardant Health: Specializing in liquid biopsies (blood tests that detect circulating tumor DNA), Guardant Health's products, like Guardant360 CDx, help monitor cancer progression and treatment response non-invasively, enabling physicians to make timely adjustments to therapy.
When and Why to Embrace This AI Application: This sophisticated ai application in healthcare is most impactful and provides the greatest value when dealing with:
- Complex diseases: Conditions like cancer, autoimmune disorders, and neurodegenerative diseases, where individual biological variability significantly impacts treatment response and outcomes.
- Rare genetic disorders: AI can help identify underlying genetic causes more quickly and match patients to emerging therapies, gene therapies, or relevant clinical trials.
- Optimizing drug selection: When multiple treatment options exist, but their efficacy and side effect profiles vary widely among patients, AI can help predict the best fit.
- Minimizing adverse drug reactions: For patient populations known to be sensitive to certain medications or when prescribing drugs with significant potential side effects.
The "why" is clear: to move beyond educated guesses and population averages to truly data-driven precision. This increases the likelihood of successful treatment from the outset, reduces unnecessary patient suffering from ineffective or harmful interventions, and tailors care to the unique biological blueprint of each individual.
Actionable Tips for Getting Started or Scaling Up: For healthcare organizations, researchers, or even tech enthusiasts in the AI workflow automation space looking to delve into or expand their use of AI for personalized medicine:
- Implement Comprehensive Electronic Health Record (EHR) Systems: High-quality, structured, and interoperable data is the absolute foundation. Ensure your EHRs are robust and capable of integration with other data sources.
- Establish Partnerships with Genomic Testing Laboratories: Access to reliable, standardized, and timely genomic data is crucial. Collaborations can streamline this process and ensure data quality.
- Train Clinical Staff on Interpreting AI-Generated Recommendations: Clinicians are the end-users. They need training to understand the outputs of AI models, their limitations, and how to integrate these insights into their clinical decision-making responsibly.
- Develop Clear Protocols for Data Sharing and Patient Consent: Trust is paramount. Ensure transparent, ethical data handling practices, robust patient consent mechanisms, and compliance with privacy regulations like HIPAA or GDPR.
- Start with Well-Established Biomarkers and Use Cases: Begin by applying AI to areas with proven clinical utility (e.g., well-validated pharmacogenomic markers) before venturing into more novel or exploratory targets. This builds confidence, demonstrates value, and allows for iterative learning.
Pioneers Pushing the Boundaries: The popularization and advancement of AI in personalized medicine are driven by visionary individuals who bridge the gap between technology and clinical practice. Figures like Eric Topol (Scripps Research), a cardiologist and author championing digital medicine; Atul Butte (UCSF), known for his work in using big data for medical breakthroughs; Regina Barzilay (MIT), an AI expert applying machine learning to oncology; Daphne Koller (insitro), leveraging ML for drug discovery; and David Feinberg (Oracle Health), leading major initiatives in health data, are instrumental. They are key in showing how ai applications in healthcare are transforming personalized treatment, bringing a future of truly individualized care closer to reality.
4. Virtual Health Assistants and Chatbots
Imagine a healthcare ally available 24/7, ready to answer your health questions, issue medication reminders, or help schedule appointments. This is the rapidly expanding reality with Virtual Health Assistants (VHAs) and AI-powered chatbots, a pivotal example of AI applications in healthcare. They're revolutionizing patient interaction by offering immediate, accessible support, acting as a friendly digital gateway to health information and basic care guidance.
What are Virtual Health Assistants and Chatbots, and How Do They Work?
At their heart, Virtual Health Assistants and chatbots are sophisticated AI-driven software programs designed to simulate human-like conversations and provide healthcare-related support. They operate using a powerful combination of Artificial Intelligence, particularly Natural Language Processing (NLP) which allows them to understand user queries (whether typed or spoken), and Machine Learning (ML) which helps them learn from countless interactions to improve their responses over time. When you interact with one, the NLP deciphers your intent, the system consults its vast knowledge base (which can include medical literature and symptom databases), and then it formulates a relevant and understandable response.
Key capabilities of these systems often include:
- Symptom Assessment & Triage: Guiding users through a series of questions to assess their symptoms and suggest potential next steps, such as self-care, consulting a pharmacist, or seeing a doctor.
- Medication Management: Offering timely reminders for medications and helping patients track their adherence, which is crucial for effective treatment.
- Appointment Scheduling: Integrating with clinic systems to help users book, reschedule, or cancel appointments, often sending automated reminders.
- Basic Medical Guidance: Answering common health questions and providing reliable information on various conditions or wellness topics.
- Mental Wellness Support: Some specialized chatbots are designed to offer emotional support, mood tracking, and coping strategies, making mental health resources more accessible.
By automating these interactions, VHAs and chatbots significantly boost patient engagement and can reduce the administrative burden on human healthcare providers, allowing them to focus on more complex patient needs.
Why Virtual Health Assistants and Chatbots Deserve Their Spot
In the rapidly evolving landscape of AI applications in healthcare, Virtual Health Assistants and chatbots stand out for their immense democratizing potential. They directly address some of healthcare's most persistent challenges: accessibility, cost, and practitioner workload. Their ability to provide 24/7 support means patients aren't limited by clinic hours for basic inquiries or guidance. Furthermore, they can scale to serve large populations, including those in remote or underserved areas, offering a vital first point of contact where direct medical access might be scarce. This immediate, often free, initial touchpoint significantly lowers barriers to seeking health information, making VHAs a cornerstone of modern, responsive healthcare.
Key Features and Benefits in Action
The sophisticated features of these AI tools translate into tangible benefits for both patients and healthcare systems:
- Natural Language Understanding: This is critical for user adoption. Instead of rigid menus, users can communicate naturally, making the interaction feel more personal and less like interacting with a machine.
- Symptom Checker & Triage Capabilities: Imagine feeling unwell late at night. A VHA can help you understand if your symptoms warrant an emergency visit or if you can wait to contact your doctor. This intelligent triage can prevent unnecessary ER visits and guide patients efficiently.
- Medication Management and Adherence Tracking: Forgetting medication is a common issue. VHAs send timely reminders and can track adherence, directly contributing to better health outcomes, especially for patients with chronic conditions.
- Efficient Appointment Scheduling and Reminder Systems: This automates a time-consuming task, freeing up clinic staff and reducing costly no-shows through automated reminders.
- Integration with Wearable Devices and Health Apps: Many VHAs can connect with data from fitness trackers or other health apps, providing a more holistic view of a user's health and enabling more personalized advice.
The overarching benefits are clear: increased patient engagement, significantly reduced wait times for common questions, improved medication adherence leading to better treatment efficacy, and cost-effective, scalable healthcare access.
Examples of Successful Implementation
Several pioneering companies highlight the real-world value of VHAs and chatbots in healthcare:
- Babylon Health (led by Ali Parsa): Known for its AI-powered symptom checker, Babylon also offers virtual consultations, efficiently triaging patients to the appropriate care pathway.
- Ada Health (co-founded by Daniel Nathrath): Ada provides a highly personalized health assessment app. Users input symptoms, and Ada’s AI asks intelligent follow-up questions to provide a detailed report, helping users make informed next steps.
- Woebot (founded by Alison Darcy): This innovative chatbot focuses on mental health, using principles of Cognitive Behavioral Therapy (CBT) to offer support, track mood, and teach coping mechanisms.
- K Health (co-founded by Allon Bloch): K Health leverages AI to compare users' symptoms against millions of anonymized medical records, offering insights into potential conditions and connecting users to affiliated doctors.
- Infermedica (co-founded by Piotr Orzechowski): This platform provides AI-driven tools for medical triage, symptom checking, and pre-diagnosis support, often integrated into existing healthcare provider systems.
These examples showcase the diverse and impactful ways AI applications in healthcare, specifically VHAs, are enhancing patient care.
Pros and Cons
While incredibly promising, it's important to have a balanced view of VHAs:
Pros:
- 24/7 Availability: Patients can access support anytime, anywhere.
- Reduced Wait Times: Immediate answers for basic health inquiries.
- Cost-Effective Engagement: Automates routine interactions, saving healthcare resources.
- Improved Medication Adherence: Timely reminders contribute to better treatment outcomes.
- Scalable Healthcare Access: Extends reach to remote or underserved populations.
Cons:
- Limited Complexity Handling: Not equipped for severe, complex, or emergency medical situations; they cannot replace a doctor's nuanced judgment.
- Risk of Misdiagnosis: AI is not infallible; incorrect advice or triage is a potential risk if not carefully designed and monitored.
- Patient Resistance: Some individuals may be hesitant to trust AI with their health or prefer human interaction.
- Privacy Concerns: Collection of sensitive health data demands robust security and adherence to regulations like HIPAA.
- Liability Issues: Determining responsibility if an AI provides incorrect medical guidance is an evolving legal area.
When and Why to Use This Approach
VHAs and chatbots are best utilized as a complementary tool within the broader healthcare ecosystem.
- Use them for: Initial patient contact and triage, answering frequent basic questions, medication reminders, chronic disease management support, mental health check-ins, and disseminating public health information efficiently.
- The "why" is compelling: They enhance patient access and convenience, improve operational efficiency for providers, can lower overall healthcare costs by guiding appropriate resource use, empower patients in their health journey, and free up human healthcare professionals for more complex cases where their expertise is most critical.
Actionable Tips for Implementation and Use
If you're considering developing, implementing, or even just using healthcare AI tools, keep these tips in mind:
- Clearly Communicate AI Limitations: Always be transparent with users that the VHA is an AI tool, not a human doctor, and has specific boundaries.
- Implement Robust Escalation Protocols: Ensure there's a seamless and quick way for users to connect with a human healthcare provider if the AI cannot handle the query or if the situation warrants it.
- Regularly Update Knowledge Bases: Medical knowledge evolves rapidly. The AI's information must be kept current with the latest medical guidelines and research.
- Prioritize Data Security and HIPAA Compliance: Protecting patient data is paramount. Ensure all systems meet strict privacy and security standards.
- Design User-Friendly Interfaces: Make the tool easy and intuitive for everyone, regardless of their tech-savviness, considering accessibility for diverse patient populations.
- Iterate and Improve: For those building these tools (even hobbyists exploring with platforms like Replit for backend logic, or n8n/Zapier for workflow automation), start with a focused scope, continuously gather user feedback, and refine the AI's performance.
Virtual Health Assistants and chatbots are more than just a technological novelty; they are becoming integral to how we approach patient care and information dissemination. As AI technology continues to advance, their capabilities will only grow, further solidifying their place among the most transformative AI applications in healthcare. For those keen to understand how such AI tools are reshaping various sectors, including the dynamic field of healthcare, you can Learn more about Virtual Health Assistants and Chatbots and discover their broader business applications, offering insights into building the future of accessible support.
5. Predictive Analytics for Disease Prevention
Imagine a healthcare "crystal ball" that could warn us about potential health problems before they escalate. That's essentially what Predictive Analytics for Disease Prevention aims to do, and it's one of the most transformative AI applications in healthcare today. Instead of waiting for patients to get sick, AI algorithms proactively analyze vast datasets—patient histories, genetics, lifestyle habits, environmental factors, and even broad population health trends. By uncovering subtle patterns and correlations often invisible to the human eye, these AI systems can forecast potential disease outbreaks, pinpoint individuals at high risk for specific conditions, and suggest timely preventive interventions. It’s all about shifting healthcare from a reactive "fix-it-when-it's-broken" model to a truly proactive, "let's-keep-it-from-breaking" approach.
How it Works: The "Magic" Behind the Prediction
This AI "magic" isn't mystical, but rather a sophisticated, data-driven process that typically involves several key steps:
- Data Collection: The process begins by gathering massive amounts of diverse data. This can include electronic health records (EHRs), genomic data, information from wearable devices (like your fitness tracker!), environmental pollution levels, social media sentiment (useful for tracking flu outbreaks, for instance), and public health databases.
- Data Preparation & Feature Engineering: Raw data is often messy. It needs to be cleaned, standardized, and organized. Then, experts identify the most relevant pieces of information (features) from the data that are likely to predict a particular outcome.
- Model Training: This is where the AI "learns." Machine learning algorithms (such as logistic regression, random forests, or even complex neural networks) are fed the prepared data. The AI diligently looks for patterns linking certain inputs (e.g., age, blood pressure, air quality) to specific outcomes (e.g., developing heart disease, an asthma exacerbation, or a flu outbreak).
- Prediction & Validation: Once trained, the model can be given new, unseen data to make forecasts. These predictions are then rigorously tested and validated against real-world outcomes to ensure their accuracy and reliability.
- Actionable Insights: Crucially, the goal isn't just to predict an event, but to provide insights that doctors, public health officials, and even individuals can act upon to prevent illness or mitigate its impact.
Why This AI Application Deserves Its Spot
Predictive analytics for disease prevention is pivotal because it fundamentally reshapes our entire health paradigm. For centuries, medicine has largely focused on treating existing illnesses. This powerful AI application in healthcare empowers us to get ahead of the curve, enabling interventions that are often simpler, less invasive, and far more effective when implemented early. This not only leads to better individual health outcomes but also has the potential to create healthier populations and more sustainable healthcare systems. It’s about giving people more healthy years and significantly reducing the burden of chronic diseases.
Key Features Driving Proactive Health
The capabilities of predictive analytics in disease prevention are broad and impactful:
- Risk Stratification and Early Warning Systems: AI can categorize patients into different risk levels (e.g., low, medium, high risk for developing diabetes) based on their unique data profile. This allows healthcare providers to focus preventive efforts on those who need them most. Early warning systems can flag patients showing subtle signs of deterioration, like impending sepsis, often hours before human clinicians might notice.
- Population Health Monitoring and Surveillance: AI tools can continuously scan public health data, social media, news reports, and even airline travel data to detect emerging disease outbreaks or unusual health trends in real-time, enabling a rapid and coordinated response.
- Chronic Disease Progression Modeling: For patients already diagnosed with chronic conditions like kidney disease or heart failure, AI can predict how their condition is likely to progress. This helps clinicians tailor treatment plans and interventions to slow down or manage that progression more effectively.
- Hospital Readmission Prediction: AI can identify patients at high risk of being readmitted to the hospital shortly after discharge. This allows hospitals to implement targeted post-discharge care and support, preventing costly and often avoidable readmissions.
- Epidemic and Outbreak Forecasting: By analyzing various data streams, AI can predict the potential spread, scale, and timing of epidemics like influenza or even new emerging infectious diseases, giving public health agencies crucial lead time to prepare.
Pros: The Bright Side of Prediction
- Early Intervention Prevents Disease Progression: Identifying risks early means lifestyle changes, screenings, or prophylactic treatments can be initiated before a disease takes hold or becomes severe.
- Reduced Healthcare Costs Through Prevention: Preventing a disease is almost always more cost-effective than treating it, especially for chronic or acute conditions requiring long-term care.
- Improved Population Health Outcomes: Healthier individuals lead to healthier communities, reducing the overall burden of disease and leading to longer, healthier lives.
- Resource Allocation Optimization: Predictive insights help healthcare systems allocate limited resources – like staff, beds, vaccines, or screening programs – more effectively.
- Enhanced Public Health Emergency Preparedness: Early warnings of outbreaks allow authorities to mobilize resources and implement control measures more efficiently.
Cons: The Challenges to Overcome
- Requires Large, High-Quality Datasets: AI models are only as good as their training data. Biased, incomplete, or low-quality data can lead to inaccurate or unfair predictions.
- False Positives May Cause Unnecessary Anxiety: If an AI incorrectly flags a healthy person as high-risk, it can cause undue stress and lead to unnecessary tests.
- Algorithmic Bias May Affect Certain Populations: If training data isn't diverse, AI models can perpetuate or amplify existing health disparities.
- Privacy Concerns with Predictive Modeling: Using sensitive personal health information raises significant privacy concerns, demanding robust data security and ethical guidelines.
- Challenges in Translating Predictions to Actionable Interventions: A prediction is useless if it doesn't lead to effective action; integrating these tools into clinical workflows is key.
Examples of Successful Implementation
We're already seeing fantastic real-world AI applications in healthcare leveraging predictive analytics:
- Epic's Sepsis Prediction Model: Integrated into many hospital EHR systems, this model helps detect early signs of sepsis, allowing for quicker treatment.
- Google's Diabetic Retinopathy Progression Prediction: AI algorithms analyze eye scans to predict the progression of diabetic retinopathy, enabling timely interventions to prevent blindness.
- Johns Hopkins' TREWS (Targeted Real-time Early Warning System): This system analyzes patient data in real-time to identify patients at high risk of developing sepsis.
- Verily's Project Baseline: A longitudinal study collecting comprehensive health data to map human health and identify predictors of disease.
- BlueDot's Infectious Disease Surveillance Platform: This Canadian company (BlueDot) famously used AI to warn its clients about the COVID-19 outbreak days before major public health organizations.
Actionable Tips for Readers: Getting Started
If you're intrigued by using predictive analytics for disease prevention, perhaps for a project or within your organization, consider these tips:
- Start with Well-Defined, High-Impact Use Cases: Don't try to boil the ocean. Focus on specific problems where predictive analytics can make a tangible difference (e.g., reducing hospital readmissions for a particular condition).
- Ensure Diverse and Representative Training Datasets: Actively work to collect and use data that reflects the diversity of the population you aim to serve. This is crucial for fairness and accuracy.
- Develop Clear Action Protocols for Positive Predictions: What happens when the AI flags a patient or situation as high-risk? There needs to be a clear, evidence-based plan for follow-up.
- Implement Continuous Model Monitoring and Updating: AI models can "drift" over time as populations and disease patterns change. They need regular evaluation and retraining.
- Collaborate with Public Health Authorities: For population-level insights and interventions, working closely with public health agencies is essential for effective implementation.
When and Why to Use This Approach
You'd want to turn to predictive analytics when your goal is to shift healthcare from being reactive to proactive. It's particularly powerful for managing population health effectively, preventing the escalation of chronic diseases like diabetes or heart disease by intervening early, bolstering public health emergency preparedness by forecasting outbreaks, and optimizing the allocation of precious healthcare resources.
The "why" is compelling: to foster healthier individuals and communities, significantly reduce the immense burden and cost of treating advanced diseases, and build more resilient and equitable healthcare systems. This powerful AI application, championed by pioneers like Kamran Khan (BlueDot), Suchi Saria (Johns Hopkins), Andrew Ng (Stanford AI), Blackford Middleton (formerly Vanderbilt), and Marzyeh Ghassemi (MIT), is a cornerstone of next-generation healthcare, heralding a future where we can more frequently stop disease before it truly starts.
6. Robotic Surgery and Surgical Assistance
Imagine a surgeon's skilled hands, but amplified – steadier, more precise, and guided by an incredibly smart co-pilot. That's the magic of AI in robotic surgery and surgical assistance, a truly game-changing area within AI applications in healthcare. This isn't about robots replacing surgeons; it's about empowering them. Sophisticated robotic systems, controlled by surgeons, offer enhanced precision and enable minimally invasive techniques. AI then adds another layer of intelligence, helping with real-time guidance, recognizing what the surgeon sees, predicting outcomes, and even learning from every procedure to get better over time.
So, how does this futuristic operating room actually function? Surgeons typically operate from a console, often in the same room, viewing a magnified 3D high-definition image of the surgical site. Their hand, wrist, and finger movements are precisely translated in real-time to the robotic arms equipped with miniaturized surgical instruments. AI supercharges this process with remarkable features:
- Unmatched precision & dexterity: AI algorithms filter out natural hand tremors and can scale the surgeon's movements. This means a large hand movement can be translated into a micro-movement inside the patient, allowing for incredibly delicate tasks that might be beyond human physical limits.
- Real-time tissue recognition and guidance: Think of it as an intelligent co-pilot. Machine learning models, trained on vast datasets of surgical videos and medical images, can identify critical structures like nerves, blood vessels, or tumor margins during the surgery, providing an extra layer of safety.
- Optimized minimally invasive procedures: AI can help plan the optimal placement of tiny incisions and the trajectory of surgical instruments to minimize tissue damage. This leads to smaller scars, less pain, and quicker recovery for patients.
- Predictive surgical planning: Before the operation even begins, AI can analyze pre-operative data (like scans and patient history) to forecast potential success rates, identify risks of complications, or estimate surgery duration, assisting in better surgical strategy and patient communication.
- Haptic feedback & augmented reality (AR) integration: While early robots lacked a strong sense of touch, newer systems are incorporating haptic feedback, allowing surgeons to "feel" tissue resistance. AI also powers AR overlays, where vital information or pre-operative images can be projected directly onto the surgeon's view of the operative field – like a smart heads-up display.
The impact of AI-driven robotics in surgery is profound, earning it a prominent spot in any discussion about leading AI applications in healthcare. The benefits extend to patients, surgeons, and the healthcare system as a whole. Key advantages include:
- Reduced surgical errors and complications: The combination of enhanced precision, tremor reduction, and real-time AI guidance directly contributes to safer procedures.
- Faster patient recovery times: Minimally invasive techniques mean smaller incisions, less pain, reduced blood loss, and often shorter hospital stays, allowing patients to return to their lives sooner.
- Enhanced surgeon capabilities: Robots can perform movements with a range of motion and stability beyond human hands and don't suffer from fatigue during long, complex operations. This allows surgeons to tackle more challenging cases and potentially extend their careers.
- Improved access to surgical expertise: While still developing, telesurgery – where a surgeon operates remotely using a robotic system – holds the promise of bringing specialized surgical care to underserved or remote areas.
The field is already demonstrating remarkable success with several pioneering systems:
- The da Vinci Surgical System by Intuitive Surgical is perhaps the most well-known. It's widely used across a range of specialties, including urology, gynecology, and general surgery, for procedures like prostatectomies and hysterectomies, featuring AI-enhanced precision for complex dissection and suturing.
- The Mako robotic arm by Stryker is a star in orthopedic surgery, particularly for knee and hip replacements. AI helps create a personalized surgical plan based on the patient's CT scan, and the robotic arm assists the surgeon in executing that plan with incredible accuracy.
- The CyberKnife radiosurgery system uses a robotic arm to deliver highly focused beams of radiation to tumors anywhere in the body with sub-millimeter accuracy. AI assists in tracking tumor movement (e.g., due to breathing) and adjusting the radiation beams in real-time.
- The Mazor X robotic spine surgery platform by Medtronic aids in delicate spine surgery, offering AI-driven pre-operative planning tools and robotic guidance for placing spinal implants with enhanced safety and precision.
- Verb Surgical's digital surgery platform, a collaboration between Johnson & Johnson and Google's Verily Life Sciences, while evolving, highlighted the vision for a comprehensive surgical ecosystem integrating robotics, advanced imaging, AI-powered data analytics, and connectivity.
These pioneering systems underscore how AI is not just an add-on but an integral part of modern surgical robotics, helping to redefine what's possible in the operating room. For those keen on how AI can streamline complex medical workflows, these are prime examples. You can Learn more about Robotic Surgery and Surgical Assistance and its wider impact on boosting efficiency.
The advancement of AI in robotic surgery owes much to key innovators and leading companies. Figures like Gary Guthart, CEO of Intuitive Surgical (home of the iconic da Vinci system, often personified or associated with 'Freddie Intuitive'), have been instrumental in popularizing robotic surgery. The teams at Verily Life Sciences (part of Alphabet) have pushed the boundaries of AI and data in surgery. Innovators such as John Mattingly of Mazor Robotics (now part of Medtronic) advanced robotic applications in spinal surgery, and Scott Huennekens, formerly of Verb Surgical, championed the vision of a digitally integrated surgical future. Their collective efforts have been crucial in translating these advanced AI applications in healthcare from research labs to real-world operating rooms.
Despite the impressive advancements and clear benefits, adopting AI in robotic surgery isn't without its hurdles and considerations:
- Extremely high equipment and maintenance costs: These systems represent a significant capital investment, often running into millions of dollars, plus ongoing service fees.
- Extensive training requirements for surgical teams: Surgeons, nurses, and technicians need specialized, lengthy training to become proficient and ensure patient safety.
- Potential for technical failures during critical procedures: Like any advanced technology, there's a risk of malfunction. Robust backup plans and emergency protocols are absolutely crucial.
- Limited tactile feedback compared to traditional surgery: While improving with haptics, the sense of touch transmitted through robotic arms may not yet fully replicate what surgeons feel directly, though AI is helping to bridge this gap.
- Potential job displacement or role shift concerns for surgical staff: While widespread displacement is unlikely, roles may evolve, requiring new skills and adaptability from the entire surgical team.
AI-assisted robotic surgery is particularly valuable and indicated when:
- Utmost precision is critical for intricate procedures in confined anatomical spaces, like in neurosurgery or delicate cancer operations.
- Minimally invasive methods are strongly preferred to reduce patient trauma, minimize scarring, and significantly speed up recovery.
- Surgeon endurance is a factor during particularly long and complex operations, where the robot can mitigate physical strain.
- Standardization and data-driven improvements are key goals, as AI can help analyze performance data from numerous surgeries to identify best practices and continuously refine techniques. This technology represents a significant leap forward in making many types of surgery safer, more effective, and less taxing on patients.
For healthcare institutions or even AI enthusiasts intrigued by implementing such advanced AI applications in healthcare, here are some practical tips:
- Invest in comprehensive surgeon and staff training programs: Thorough, continuous training, including simulation and proctoring, is paramount for safety and achieving optimal outcomes.
- Start with less complex procedures before advancing: Gradually introduce robotic surgery, beginning with procedures where the benefits are clear and the learning curve is manageable for the team.
- Establish robust maintenance and technical support protocols: Ensure immediate access to technical support and a proactive maintenance schedule to minimize downtime and critical risks.
- Implement quality assurance and outcome tracking systems: Continuously monitor surgical outcomes, patient recovery rates, and any complications to refine techniques, demonstrate value, and ensure ongoing improvement.
- Consider leasing options or strategic partnerships to manage high upfront costs: This can make the technology more accessible, especially for smaller institutions or those wanting to pilot the technology.
7. Mental Health and Behavioral Analysis
The mind's complexities present unique challenges for healthcare, but AI applications in healthcare are increasingly stepping up to offer innovative support for mental health and behavioral analysis. This rapidly evolving field uses intelligent systems to understand our emotional states, identify behavioral patterns, and provide accessible support, often directly through the smartphones and devices we use every day. It's about leveraging the power of artificial intelligence to make mental wellness more attainable, personalized, and proactive for everyone.
How Does AI Lend a Digital Ear and a Helping Hand?
At its heart, AI in mental health operates by processing diverse data types—from text and voice to behavioral cues—to learn, spot patterns, and deliver personalized interactions. This isn't about replacing human therapists but augmenting their reach and providing new avenues for support. Let's look at some of the key features driving this revolution:
- Mood and Behavior Pattern Recognition: Imagine an app that, with your permission, learns your typical communication style, activity levels, or even sleep patterns. AI algorithms can analyze this data to detect subtle deviations that might indicate a shift in mood or the early signs of a mental health concern like depression or anxiety. This feature can act as an early warning system, prompting self-reflection or professional consultation.
- Natural Language Processing (NLP) for Therapy Sessions: This is where AI truly starts to "listen" and "understand." NLP enables AI-powered chatbots and virtual therapists to comprehend and respond to human language in a surprisingly nuanced way. You can type or speak your feelings, and the AI can identify key themes, reflect sentiments, and even guide you through structured therapeutic exercises based on established techniques like Cognitive Behavioral Therapy (CBT).
- Digital Therapeutic Interventions: These are essentially AI-driven, evidence-based treatment programs delivered via apps or web platforms. Think guided meditations tailored to your stress levels, interactive modules to help you challenge negative thought patterns, or structured plans to build better coping skills. These interventions can be accessed on-demand, offering consistent support whenever needed.
- Suicide Risk Assessment and Prevention: This is a critical and highly sensitive application. AI systems can be trained to analyze language patterns (in text or speech) or behavioral shifts that are statistically associated with an increased risk of suicide. While not a standalone diagnostic tool and never a replacement for human judgment, it can flag individuals who might need immediate, urgent intervention from human professionals or crisis services.
- Personalized Mental Health Recommendations: Based on all the data it ethically gathers and the patterns it recognizes, AI can suggest tailored resources, coping strategies, articles, or activities. It can also intelligently recommend when it might be beneficial for an individual to connect with a human therapist for deeper support.
Why AI in Mental Health is a Pivotal Advancement
The integration of AI into mental health services isn't just a technological novelty; it's a significant leap forward for AI applications in healthcare because it directly addresses longstanding challenges in mental wellness:
- It dramatically boosts increased access to mental health support, especially for those in remote areas, with mobility issues, or facing long wait times for traditional services.
- AI platforms can lead to reduced stigma as many individuals feel more comfortable initially discussing sensitive mental health issues with an anonymous and non-judgmental digital interface.
- The capability for continuous monitoring and early intervention is a game-changer. Unlike sporadic therapy sessions, AI can offer ongoing, subtle tracking, potentially allowing for the detection of issues at their nascent stages.
- These tools often provide cost-effective therapy alternatives or valuable supplements to traditional care, making support more affordable.
- AI can contribute to a more objective assessment of mental health status over time by providing data-driven insights into mood trends and behavioral changes, which can complement a therapist's observations.
These benefits underscore why AI in mental health is a crucial development, paving the way for more inclusive, responsive, and personalized care.
Pioneers Paving the Way: Real-World Examples
Several innovative platforms are already demonstrating the profound impact of AI in the mental health space:
- Woebot: Founded by psychologist Alison Darcy, Woebot is a popular AI chatbot that uses principles of Cognitive Behavioral Therapy (CBT) to help users manage their mood, reduce stress, and learn effective coping skills through empathetic, interactive conversations.
- Ginger: Led by CEO Karan Singh, Ginger offers an on-demand mental health platform that intelligently combines AI-powered coaching and behavioral health tracking with access to human therapists and psychiatrists, providing a comprehensive care model.
- Lyra Health: Co-founded by David Ebersman, Lyra Health utilizes AI to power its therapy matching system, connecting individuals with the most suitable mental health providers and evidence-based treatments based on their specific needs and preferences.
- Ellipsis Health: This pioneering company is at the forefront of using AI to analyze speech patterns—the acoustic and linguistic features of a person's voice—as a vital sign for mental health, enabling early and objective screening for conditions like depression and anxiety.
- X2AI (Tess): This platform provides AI-enhanced therapy tools, offering personalized psychological support through empathetic, AI-driven conversations. Tess aims to make mental healthcare more accessible, affordable, and available 24/7.
The visionary work of young AI advocates like Tanmay Bakshi, who champions AI for social good including mental health, and foundational researchers like Professor Rosalind Picard of MIT, a pioneer in Affective Computing (AI that recognizes, interprets, processes, and simulates human emotions), continues to inspire and fuel innovation in this vital area.
Navigating the Digital Couch: Pros and Cons
While the potential of AI in mental health is immense, it's crucial to approach it with a balanced perspective, acknowledging both its strengths and current limitations:
Pros:
- Significantly broadens access to mental health support.
- Lowers stigma associated with seeking help through anonymous digital engagement.
- Enables continuous monitoring, facilitating early detection and intervention.
- Offers cost-effective alternatives or valuable supplements to traditional therapy.
- Can provide objective data points for assessing and tracking mental health status over time.
Cons:
- AI cannot replicate genuine human empathy, the depth of nuanced understanding, or the critical therapeutic alliance that forms the core of many successful therapies.
- Significant privacy and data security concerns exist regarding the collection, storage, and use of highly sensitive personal mental health data.
- There's a risk of misdiagnosis or inappropriate advice, especially in complex mental health conditions, if AI systems are not robustly validated and carefully implemented.
- Current AI tools may have limited effectiveness for severe psychiatric disorders that require intensive human intervention, comprehensive care plans, and often medication.
- There's a potential for users to become overly dependent on technology for emotional support, possibly neglecting real-world relationships or the need for deeper professional help.
When and Why to Embrace AI in Mental Health
AI-driven mental health tools are particularly valuable in specific contexts:
- For Early Exploration and Support: When someone is hesitant to see a human therapist or simply wants to understand their feelings better in a private, non-judgmental setting.
- As a Supplement to Traditional Therapy: To reinforce concepts learned in sessions with a human therapist, practice coping skills consistently, or track mood and progress between appointments.
- To Bridge Gaps in Access: In geographical areas with a shortage of mental health professionals or for individuals facing financial, mobility, or time constraints.
- For Ongoing Maintenance and Well-being: To promote daily mental wellness practices, build resilience, and manage everyday stressors, much like using an app for physical fitness.
The "why" is compelling: these tools empower individuals by providing immediate, personalized, and often judgment-free support. They can help shift mental healthcare from a reactive model to a more proactive one, integrating seamlessly into the digital lives many people already lead. This proactive and personalized approach is a hallmark of many beneficial AI applications in healthcare.
Actionable Tips for Responsible Integration
For those building, implementing, or considering the use of these AI tools, responsible deployment is paramount:
- Ensure Licensed Mental Health Professionals Oversee AI Systems: Their expertise is crucial for clinical validity, safety, and ethical considerations.
- Implement Robust Crisis Intervention Protocols: Platforms must have clear, effective protocols for high-risk situations, including immediate pathways to connect users with human emergency services or support lines.
- Use Validated Psychological Assessment Tools and Therapeutic Techniques: Ensure the AI's methods are grounded in evidence-based practices.
- Maintain Transparency About AI Capabilities and Limitations: Users should always be aware they are interacting with an AI and understand what it can and cannot do.
- Provide Seamless Escalation to Human Therapists When Needed: Make it easy and clear for users to transition to human support if the AI is insufficient, or if they simply prefer human interaction.
The journey of integrating AI into mental health care is dynamic and full of promise. As these technologies mature, their role within the broader landscape of AI applications in healthcare will undoubtedly expand, offering new hope and innovative solutions for understanding, supporting, and enhancing our collective mental well-being. The key will be to foster a synergy where AI augments and supports, rather than attempts to replace, the invaluable human element of care.
8. Electronic Health Records and Clinical Decision Support
Imagine a world where your doctor's notes don't just sit in a digital file but actively work to keep you healthier. That's the power AI brings to Electronic Health Records (EHRs) and Clinical Decision Support (CDS) systems, making this one of the most impactful ai applications in healthcare today. EHRs are the digital versions of patients' paper charts, holding their medical history. CDS systems, on the other hand, are tools designed to provide clinicians with specific knowledge and patient information, intelligently filtered and presented at the right times, to enhance health and healthcare delivery. When AI enters this equation, these systems transform from passive data repositories into intelligent, proactive assistants for healthcare professionals, truly revolutionizing how care is managed and delivered.
How AI Transforms EHRs and CDS
So, how does AI weave its magic into EHRs and CDS? It primarily leverages two powerful branches of artificial intelligence: Natural Language Processing (NLP) and Machine Learning (ML).
NLP is a game-changer because it allows computers to understand and process human language. In healthcare, this means AI can read and interpret the vast amounts of unstructured data in clinical notes – the detailed narratives, observations, and histories doctors write. Information that was previously "locked" in text can now be extracted, analyzed, and made actionable.
Machine Learning algorithms then take center stage by sifting through colossal datasets, including structured data (like lab results and diagnoses) and NLP-extracted insights. These ML models can identify complex patterns, predict potential health risks (like the likelihood of a patient developing a specific condition), and uncover correlations that would be virtually impossible for humans to detect on their own.
This AI integration powers a suite of transformative features:
- Automated Clinical Documentation and Coding: AI can assist in generating clinical notes from doctor-patient conversations (ambient clinical intelligence) or suggest accurate medical codes for billing, significantly reducing administrative burdens.
- Real-time Alerts: Intelligent systems can flag critical issues like potential drug interactions, allergies, abnormal lab values, or signs of patient deterioration, providing immediate warnings to clinicians.
- Evidence-Based Treatment Recommendations: By analyzing a patient's specific data against the latest medical research, clinical guidelines, and outcomes from similar patient populations, AI can suggest personalized and evidence-based treatment options.
- Clinical Workflow Optimization: AI automates routine tasks, prioritizes information, and streamlines processes, allowing clinicians to dedicate more time to direct patient care and complex decision-making.
- Population Health Analytics: AI tools can analyze anonymized data from entire patient populations to identify health trends, predict disease outbreaks, manage chronic conditions more effectively, and inform public health strategies.
Why AI-Powered EHRs and CDS Deserve the Spotlight
The integration of AI into EHR and CDS systems isn't just an incremental improvement; it's a fundamental leap forward that firmly establishes its place among essential ai applications in healthcare. This is because it directly tackles some of the most pressing challenges in modern medicine, including information overload, clinician burnout, and the quest for safer, more personalized care.
The benefits are compelling and far-reaching:
- Reduced Administrative Burden on Clinicians: AI takes over time-consuming tasks like data entry and chart review, freeing up clinicians to focus on what they do best – caring for patients.
- Improved Clinical Decision-Making: With AI providing tailored, evidence-based insights at the point of care, clinicians are better equipped to make accurate diagnoses and choose the most effective treatment plans.
- Enhanced Patient Safety: AI-driven alerts for drug interactions, allergies, or deteriorating conditions act as a crucial safety net, helping to prevent medical errors and improve patient outcomes.
- Better Care Coordination: AI facilitates standardized documentation and seamless sharing of relevant information, improving communication and collaboration among multidisciplinary care teams.
- Standardized and Higher Quality Clinical Documentation: AI can prompt for missing information and ensure records are more complete and consistent, which is vital for continuity of care, research, and quality improvement.
Examples of Successful Implementation
We're already witnessing the tangible impact of AI-enhanced EHR and CDS systems in real-world healthcare settings.
- Epic Systems, founded by Judy Faulkner, is a leading EHR provider that has embedded AI tools to assist with tasks like predicting sepsis risk, identifying patients who might benefit from early interventions, and streamlining charting.
- Cerner (whose late founder Neal Patterson was a visionary in health IT) offers platforms like HealtheLife that utilize AI for population health management, helping organizations analyze data to improve community health outcomes.
- IBM Watson Health, while having evolved its focus, was an early pioneer in applying AI to clinical decision support, particularly in oncology, by analyzing vast amounts of medical literature and patient data.
- Allscripts integrates AI into its EHR systems to enhance workflow efficiency and provide clinicians with actionable insights.
- Specialized AI tools are also making waves. For example, Veracyte's genomic classifiers integrate with EHRs to provide physicians with advanced diagnostic insights for conditions like thyroid and lung cancer, directly within their existing workflows.
When and Why to Embrace This AI Approach
Healthcare organizations looking to significantly elevate their performance and patient care should strongly consider integrating AI into their EHR and CDS strategies. This approach is particularly beneficial when aiming to:
- Boost operational efficiency and reduce clinician burnout.
- Improve diagnostic accuracy and personalize treatment protocols.
- Proactively enhance patient safety and minimize preventable medical errors.
- Effectively manage the health of large patient populations and identify at-risk individuals.
- Support clinicians in navigating the ever-expanding universe of medical knowledge.
The core "why" is compelling: The sheer volume, velocity, and variety of medical data generated daily are far beyond human capacity to process comprehensively. AI acts as an indispensable cognitive partner, sifting through this data deluge to find critical signals, ensuring decisions are informed by the most complete and current evidence. This is a vital component of modernizing healthcare delivery.
Actionable Tips for Implementation and Optimization
If you're involved in or simply curious about leveraging AI in EHR and CDS, or even building AI-powered workflows in other domains, here are some key tips for success:
- Customize Alert Systems Thoughtfully: A common pitfall is "alert fatigue," where clinicians become desensitized by excessive notifications. It's crucial to tailor alerts to be highly relevant and minimize noise, ensuring that truly critical warnings are heeded.
- Invest in Comprehensive Staff Training: New AI tools can initially disrupt established workflows. Thorough training, ongoing support, and involving clinicians in the design and refinement process are essential for smooth adoption and effective utilization. As you develop or implement these systems, understanding how to frame your queries or instructions to the AI can also be crucial. For example, effective prompt engineering can significantly boost AI's performance in extracting insights or generating summaries. You can Learn more about Electronic Health Records and Clinical Decision Support and discover techniques to refine your interactions with AI for better outcomes.
- Prioritize Robust Data Security and Privacy: Patient data is exceptionally sensitive. Implementing stringent security measures, ensuring compliance with regulations like HIPAA (in the US), and having reliable data backup and disaster recovery plans are non-negotiable.
- Plan for Interoperability: Healthcare is a collaborative endeavor. Strive for AI solutions that can communicate and share data effectively with other healthcare IT systems (both internal and external) to ensure seamless care coordination and avoid data silos.
- Continuously Monitor and Iterate: After deployment, keep a close watch on system performance, user satisfaction, and, most importantly, clinical outcomes. Be prepared to make adjustments, refine algorithms, and iterate on workflows based on real-world feedback and performance data.
Acknowledging the Pros and Cons
The advantages of AI-infused EHRs and CDS are transformative: less administrative work for clinicians, sharper data-driven decision-making, heightened patient safety via automated alerts, and smoother care coordination.
However, it's important to navigate potential challenges:
- Alert Fatigue: As noted, poorly configured alerts can overwhelm users.
- Integration Challenges: Marrying new AI systems with existing legacy IT infrastructure can be complex and costly.
- High Implementation Costs: The initial investment in technology, training, and change management can be substantial.
- Workflow Disruption: The transition period requires careful management to minimize disruption and ensure buy-in.
- Vendor Lock-in and Interoperability: Dependence on a single vendor or difficulties in data exchange with other systems can pose long-term issues.
Despite these challenges, the trajectory is clear. The fusion of AI with Electronic Health Records and Clinical Decision Support represents a monumental step forward in making healthcare smarter, safer, and more efficient. The ongoing innovation in this field, championed by thought leaders such as medical informaticist David McCallie, healthcare IT leader Blackford Middleton, and John Mattison (formerly Kaiser Permanente CIO), ensures that these ai applications in healthcare will only become more sophisticated and indispensable in the years to come.
9. Medical Research and Clinical Trials
Medical research and clinical trials form the backbone of healthcare progress, but they're notoriously slow, incredibly expensive, and often fraught with complexity. Traditionally, bringing a new drug or therapy to market can take over a decade and cost billions. This is where AI steps in, offering a revolutionary shift and establishing itself as one of the most transformative ai applications in healthcare. It's not just about making things faster; AI is making medical research smarter, more efficient, and ultimately, more focused on the patient.
How AI is Reshaping Research and Trials
AI achieves this paradigm shift through a powerful suite of interconnected capabilities, fundamentally altering how studies are designed, executed, and analyzed:
- Automated Literature Review and Synthesis: Imagine researchers manually sifting through thousands of scientific papers. AI, particularly leveraging Natural Language Processing (NLP), can accomplish this in a fraction of the time. It scans, comprehends, and synthesizes information from vast databases of research papers, patents, and existing clinical trial data. This rapid analysis helps pinpoint knowledge gaps, identify potential drug targets, and spot emerging scientific trends far more quickly.
- Intelligent Patient Recruitment and Matching: One of the biggest hurdles in clinical trials is finding and enrolling the right participants. AI algorithms excel at analyzing extensive datasets, including anonymized electronic health records (EHRs), genomic information, and other relevant data sources, to identify eligible patients who meet complex inclusion and exclusion criteria. This dramatically accelerates enrollment, reduces a common bottleneck, and ensures a better match between the patient and the trial's objectives.
- Protocol Optimization and Adaptive Trial Design: Crafting an effective clinical trial protocol is an intricate task. AI can simulate various trial designs, predict potential challenges, and even suggest modifications to optimize the study's structure. This has given rise to 'adaptive trial designs,' where protocols can be adjusted in real-time based on incoming data, increasing the trial's efficiency and chances of success.
- Real-World Evidence (RWE) Generation: Beyond controlled trials, AI is instrumental in analyzing real-world data – information gathered from everyday healthcare interactions, such as EHRs, patient registries, and even wearable devices. This RWE provides crucial insights into how treatments perform across diverse, real-life patient populations, complementing traditional trial findings and offering a more comprehensive view of a therapy's effectiveness and safety.
- Clinical Trial Outcome Prediction: Before significant resources are committed, or even during the early phases of a trial, machine learning models can analyze preliminary data, patient characteristics, and other influencing factors to forecast the likelihood of a trial's success. This predictive capability allows researchers to prioritize the most promising avenues, potentially re-directing resources or halting unpromising trials earlier, thus saving valuable time and investment.
The collective impact of these AI-driven features is profound. We are witnessing faster trial enrollment and completion, leading to quicker patient access to innovative treatments. There's a significant potential for reduced clinical trial costs, freeing up resources for further research. Improved patient matching not only enhances the probability of trial success but can also lead to better outcomes for individual participants. Moreover, AI facilitates enhanced safety monitoring during trials by rapidly detecting potential adverse events. The culmination of these advancements is the acceleration of drug discovery and faster approval processes, bringing life-saving therapies to the market sooner.
Why AI in Research Deserves a Spotlight
Medical research and clinical trials are quite literally the engine of medical progress. Any technology capable of fundamentally improving the speed, cost-effectiveness, and success rate of this engine has far-reaching implications for global health. AI is doing precisely that, moving beyond incremental improvements to offer a paradigm shift in how we discover, develop, and validate new therapies. This particular one of the ai applications in healthcare is so vital because it directly influences how rapidly we can address diseases, alleviate suffering, and enhance the quality of life for millions.
Pioneering Examples in Action
The application of AI in this field is not just a futuristic concept; it's happening now, with leading organizations making significant strides:
- Deep 6 AI, co-founded by Wout Brusselaers, utilizes sophisticated AI to analyze complex medical records, identifying suitable patients for clinical trials in minutes – a task that traditionally could take months.
- Antidote operates a digital platform that intelligently matches patients with relevant clinical trials, empowering individuals to find and participate in research more easily.
- Trials.ai specializes in AI-powered tools that assist in designing and optimizing clinical trial protocols, aiming to enhance study efficiency right from the planning stages.
- Pharmaceutical giants like Roche and Novartis (where individuals like Rita Scichilone have been influential in AI adoption) are deeply investing in AI across their entire clinical development pipelines. Novartis, for instance, employs AI to analyze complex biological datasets for drug discovery, predict patient responses to treatments, and streamline trial operations. Figures such as Ahmad Doroudian at Genentech, and renowned experts like clinical trial innovation specialist Craig Lipset and Yale's Harlan Krumholz (a leader in outcomes research, highly relevant to RWE), have also been vocal advocates for AI's transformative potential in this space.
When and Why to Embrace AI in Research
For research institutions, biotech companies, or pharmaceutical firms, the question is when and why to integrate AI into their research and trial processes. Consider leveraging these AI-driven approaches when:
- You are managing and trying to derive insights from vast volumes of complex, often unstructured, data (e.g., genomic sequences, research publications, patient notes).
- Accelerating the research and development timeline, from initial discovery to market availability, is a critical strategic objective.
- There's a need to enhance the precision of patient selection for trials, particularly for those involving rare diseases, specific genetic markers, or highly targeted therapies.
- You are looking to mitigate the high failure rates and substantial costs typically associated with traditional clinical trials.
- The goal is to uncover novel insights, biomarkers, or patterns from existing data that might be missed by conventional human analysis.
The 'why' is compelling: AI paves the way for more personalized medicine by ensuring that the right patients are enrolled in the most appropriate trials. It boosts the efficiency of the entire research lifecycle, from foundational discovery to post-market surveillance. This allows for smarter resource allocation, minimizes waste, and ultimately increases the probability of successfully bringing beneficial new treatments to the patients who await them. The innovative spirit driving these changes is reshaping many industries. For instance, you can Learn more about Medical Research and Clinical Trials and how similar open innovation principles are applied elsewhere.
Actionable Tips for Implementation
If you're an AI enthusiast, part of a Vibe builder team, or involved in a go-to-market strategy that could leverage these ai applications in healthcare, here are some friendly, actionable tips:
- Establish Robust Data Governance: Data is the lifeblood of AI. Implement clear protocols for data quality, privacy (adhering to regulations like GDPR or HIPAA), security, and ethical data sharing, especially when handling sensitive patient information.
- Collaborate with Regulatory Agencies Early: The regulatory landscape for AI in healthcare is dynamic. Engage with bodies like the FDA (U.S. Food and Drug Administration) or EMA (European Medicines Agency) early in your development process to understand expectations and ensure a smoother pathway for validation and approval.
- Champion Diverse and Representative Data: AI models learn from the data they are fed. Actively work to ensure your datasets are diverse and representative of various demographic and clinical populations to avoid creating or perpetuating biases that could render AI tools less effective or even inequitable for certain groups.
- Implement Rigorous Quality Assurance (QA): AI-generated insights are powerful but not infallible. Develop strong validation processes, always including human oversight and clinical expertise, to verify the outputs and predictions from AI models before making critical research or clinical decisions.
- Maintain Transparency in AI Methodology: Be as clear as possible about how your AI models work, the data they utilize, and their inherent limitations. This "explainability" is crucial for building trust with researchers, clinicians, patients, and regulatory bodies.
Pros and Cons: A Balanced View
While AI offers tremendous promise for medical research and clinical trials, it's important to acknowledge both its advantages and current challenges:
Pros:
- Accelerated Timelines: Significantly faster trial enrollment, quicker study completion, and potentially expedited drug approval processes.
- Reduced Costs: Optimization of protocols, improved patient selection, and early prediction of trial failures can lead to substantial cost savings.
- Improved Patient Matching & Outcomes: More precise identification of suitable trial candidates can enhance the likelihood of positive trial results and better individual patient benefits.
- Enhanced Safety Monitoring: AI can analyze real-time data to detect adverse events or safety signals more rapidly than traditional methods.
- Deeper Insights: Streamlined discovery of novel insights, biomarkers, and correlations from complex datasets.
Cons:
- Regulatory Uncertainty: The evolving nature of regulations for AI-enhanced trials can create ambiguity for developers and sponsors.
- Risk of Algorithmic Bias: If AI models are trained on non-diverse or biased datasets, they can perpetuate or even amplify existing disparities in patient selection and outcomes.
- Limited Generalizability: AI-optimized protocols designed for a specific population or context may not be directly transferable or equally effective elsewhere without recalibration.
- High Implementation Costs: The initial investment in AI technology, infrastructure, and specialized talent can be substantial.
- Challenges in Validating Insights: Fully understanding and independently verifying why an AI model (especially complex "black box" models) arrived at a particular conclusion or prediction can be difficult, posing challenges for validation and trust.
Despite these challenges, the momentum behind AI in medical research and clinical trials is undeniable. As the technology matures and ethical frameworks evolve, AI is set to play an increasingly indispensable role in the future of how we discover, develop, and deliver life-changing medical innovations.
10. Epidemic Surveillance and Public Health Monitoring
Imagine a global network of digital sentinels, tirelessly sifting through mountains of data, listening to the whispers of the internet, and watching environmental shifts, all to catch the faintest signal of a new disease outbreak before it explodes into a worldwide crisis. This isn't science fiction; it's the reality of Epidemic Surveillance and Public Health Monitoring, one of the most impactful AI applications in healthcare today. This approach uses artificial intelligence to act as an early warning system for humanity, helping us stay one step ahead of infectious diseases.
How It Works: AI as a Digital Disease Detective
At its core, AI-powered epidemic surveillance is about connecting the dots on a massive scale. Traditional methods often rely on official reports from clinics and hospitals, which can lag days or even weeks behind an actual outbreak. AI systems, however, cast a much wider net, ingesting and analyzing a diverse array of real-time data sources. This includes:
- Official Health Data: Information from organizations like the World Health Organization (WHO) and local health departments.
- News Reports & Online Media: AI, particularly Natural Language Processing (NLP), scans articles from around the globe in multiple languages for mentions of unusual symptoms or clusters of illness.
- Social Media: Platforms like X (formerly Twitter) and local forums can provide early, albeit noisy, signals. AI analyzes posts for keywords, sentiment, and geographic clustering related to health concerns.
- Airline Ticket Data & Mobility Patterns: Understanding how people are moving helps predict how a disease might travel.
- Environmental & Climate Data: Factors like temperature changes, rainfall, and animal migration patterns can influence the emergence and spread of diseases, especially zoonotic ones (those jumping from animals to humans).
- Livestock Health Reports: Monitoring animal populations for signs of disease can provide early warnings for potential human outbreaks.
Machine learning algorithms then get to work, identifying anomalies, patterns, and correlations that human analysts might miss or take too long to find. Think of it as a super-smart detective that never sleeps, constantly looking for clues that something is amiss.
Key Features That Make a Difference:
These AI systems aren't just data vacuums; they offer sophisticated capabilities:
- Real-time Disease Outbreak Detection: Identifying unusual spikes in illness reports or symptom mentions far faster than traditional methods.
- Epidemiological Modeling and Spread Prediction: Once an outbreak is detected, AI can model how it might spread based on factors like population density, travel routes, and the disease's characteristics.
- Social Media and News Sentiment Analysis: Gauging public concern, identifying misinformation, and sometimes even picking up on unreported cases through discussions of symptoms.
- Environmental Health Factor Monitoring: Correlating environmental changes (e.g., deforestation, unusual weather) with disease risk.
- Resource Allocation Optimization: During a health emergency, AI can help public health officials decide where to send medical supplies, personnel, and testing kits most effectively.
Success Stories in Action:
The power of AI in this domain isn't just theoretical. Several platforms have demonstrated remarkable success:
- BlueDot: Founded by Dr. Kamran Khan, this Canadian company famously flagged an unusual pneumonia outbreak in Wuhan, China, on December 31, 2019 – nine days before the WHO officially announced COVID-19. BlueDot (bluedot.global) uses AI to analyze vast amounts of data, including global airline ticketing data, to track and anticipate the spread of infectious diseases.
- HealthMap: Co-created by Dr. John Brownstein, HealthMap (healthmap.org) at Boston Children's Hospital provides a global, real-time view of emerging public health threats by scouring online sources in 15 languages.
- WHO's EIOS (Epidemic Intelligence from Open Sources): This initiative (who.int/initiatives/eios) leverages open-source information, including media reports and online content, to detect and assess public health risks globally, collaborating with numerous organizations.
- Metabiota: Founded by Nathan Wolfe, this company (metabiota.com) focuses on epidemic risk modeling, helping governments and businesses understand and mitigate the impact of infectious diseases.
- Google Flu Trends (Discontinued but Influential): While eventually discontinued due to some accuracy issues, this project, involving researchers like Jeremy Ginsberg, was a pioneering effort that demonstrated the potential of using search query data to track flu outbreaks in near real-time. It highlighted both the promise and the pitfalls, teaching valuable lessons for subsequent systems. Epidemiologist Larry Brilliant, known for his work on smallpox eradication and later with Google.org, has long championed such innovative approaches to global health.
The Bright Side: Pros of AI Vigilance
The benefits of leveraging AI for epidemic surveillance are profound:
- Early Warning Systems: The potential to detect outbreaks days or weeks earlier can prevent them from escalating into large-scale epidemics or pandemics.
- Rapid Response Coordination: Quicker detection allows for faster mobilization of resources, contact tracing, and public health interventions, ultimately saving lives.
- Improved Pandemic Preparedness: Continuous global surveillance helps identify vulnerabilities and strengthens our collective ability to respond to future threats.
- Data-Driven Policy Making: AI provides public health officials with robust data to inform decisions on travel restrictions, vaccination campaigns, and resource allocation.
- Cost-Effectiveness: Automated monitoring can be more efficient and less resource-intensive than relying solely on traditional manual surveillance methods.
Navigating the Challenges: Cons to Consider
Despite its immense potential, this AI application in healthcare comes with challenges:
- Privacy Concerns: Collecting and analyzing population-level data, even anonymized, raises legitimate privacy questions.
- False Alarms: AI systems can sometimes flag anomalies that turn out to be benign, potentially causing unnecessary panic or resource diversion.
- Data Quality and Availability: The effectiveness of these systems heavily depends on the quality, quantity, and accessibility of data, which can vary significantly across regions.
- Challenges in International Coordination: Diseases don't respect borders, but international data sharing and coordinated response efforts can be complex.
- Potential for Misuse: There's a risk that surveillance technologies could be repurposed by governments for unauthorized monitoring or control.
Actionable Tips for Harnessing This Power:
For those looking to understand or contribute to this field, or for policymakers implementing such systems:
- Integrate Diverse Data Sources: The more comprehensive the data, the more accurate the insights. Combine official reports with unstructured data like news and social media.
- Establish Clear Protocols for Outbreak Response: AI can raise the alarm, but human-led response plans must be in place to act on the information effectively.
- Collaborate with International Health Organizations: Global health security is a shared responsibility. Partnerships are key to effective surveillance and response.
- Ensure Transparency in Data Collection and Usage: Build public trust by being open about what data is collected, how it's used, and the safeguards in place.
- Maintain Human Oversight: AI should augment, not replace, human expertise. Public health experts must validate AI-generated alerts and guide decision-making.
When and Why to Use This AI Superpower
This AI-driven approach is crucial for:
- Early detection of novel or re-emerging pathogens.
- Tracking the real-time spread of known diseases (e.g., flu, measles, Ebola).
- Informing timely and targeted public health interventions.
- Efficiently allocating scarce resources during health emergencies.
- Understanding disease dynamics to improve epidemiological models.
- Strengthening national and global pandemic preparedness infrastructures.
Ultimately, AI-powered epidemic surveillance and public health monitoring represents a significant leap forward in our ability to protect global health. By intelligently analyzing the world's data, these systems provide an invaluable early warning capability, making them one of the most vital AI applications in healthcare for a safer, healthier future.
AI Healthcare Applications Comparison Matrix
| Application Area | Implementation Complexity 🔄 | Resource Requirements ⚡ | Expected Outcomes 📊 | Ideal Use Cases 💡 | Key Advantages ⭐ |
|---|---|---|---|---|---|
| Medical Imaging and Diagnostics | High due to data needs and regulatory | Extensive annotated image datasets, HPC | Improved diagnostic accuracy, faster image analysis | Early-stage disease detection, emergency diagnostics | Higher accuracy than humans, 24/7 availability |
| Drug Discovery and Development | Very high, combines AI with lab validation | High computational power, chemical data | Reduced discovery timeline, cost savings | Target ID, compound optimization, drug repurposing | Faster R&D, tackles undruggable targets |
| Personalized Treatment and Precision Medicine | High complexity integrating varied data | Genomic data, patient history, biomarkers | Better treatment efficacy, fewer side effects | Tailored therapies, rare diseases | Improved outcomes, cost-effective targeted care |
| Virtual Health Assistants and Chatbots | Moderate, NLP and system integration | Cloud infrastructure, conversational AI | 24/7 patient support, symptom triage | Patient engagement, medication adherence | Scalable, reduces provider workload |
| Predictive Analytics for Disease Prevention | High, requires large datasets and modeling | Big data, EHR integration, analytics tools | Early intervention, reduced hospitalizations | Disease outbreaks, chronic condition management | Preventive care, resource allocation optimization |
| Robotic Surgery and Surgical Assistance | Very high, involves hardware and software | Specialized robotic devices, training | Reduced errors, faster recovery | Minimally invasive surgery, precision procedures | Enhanced surgeon dexterity, less invasive surgery |
| Mental Health and Behavioral Analysis | Moderate, focused on sensitive data | NLP models, continuous monitoring tools | Increased access to therapy, early detection | Digital therapeutics, behavioral monitoring | Reduced stigma, scalable mental health support |
| Electronic Health Records and Clinical Decision Support | High due to system integration and training | EHR software, NLP, clinical data | Reduced clinician workload, improved decisions | Clinical documentation, alerts, population health | Improved safety, workflow optimization |
| Medical Research and Clinical Trials | High, handling complex data and protocols | Data analytics, patient datasets | Faster trials, cost reduction, better patient matching | Protocol design, patient recruitment, outcome prediction | Accelerated research, lower costs |
| Epidemic Surveillance and Public Health Monitoring | High, requires multi-source integration | Real-time data streams, analytics engines | Early outbreak detection, rapid public health response | Global disease tracking, emergency preparedness | Early warnings, cost-effective surveillance |
The Future is Now: Embracing AI in Healthcare
As we've journeyed through the incredible landscape of ai applications in healthcare, from sharpening medical imaging and accelerating drug discovery to personalizing treatment plans and empowering virtual health assistants, one thing is crystal clear: the future of medicine is not just knocking on our door, it’s already stepping inside. The ten areas we've explored highlight a profound shift towards a healthcare system that's more efficient, remarkably precise, and deeply personalized, all thanks to the power of artificial intelligence.
The most important takeaway is that these ai applications in healthcare are rapidly moving from experimental phases to real-world solutions, delivering tangible benefits to patients and practitioners alike. For AI enthusiasts, hobbyist builders, and those looking to automate workflows or explore innovative use cases with tools like LLMs, Replit, n8n, or Zapier, understanding these advancements is incredibly valuable. It’s about grasping how technology can solve complex problems, improve lives, and open up new avenues for innovation and contribution.
Embracing these concepts means being part of a wave that's enhancing diagnostic accuracy, making drug development faster, tailoring treatments to individual needs, and even helping us predict and manage public health crises more effectively. The broader impact is undeniable: a healthier future for everyone, driven by intelligent insights and collaborative breakthroughs. The journey of AI in medicine is ongoing, fueled by continuous learning and a shared passion for progress.
Feeling inspired by the transformative potential of ai applications in healthcare? If you're keen to dive deeper, connect with fellow AI explorers, or start building your own innovative projects, VibeMakers is a vibrant community designed for you. It's the perfect place to find resources, share ideas, and collaborate with others who are just as excited about shaping the future of AI, including its incredible impact on health and well-being.